Aging is a significant risk factor for ischemic stroke and worsens its outcome. However, the mechanisms for this worsened neurological outcome with aging are not clearly defined. In a study led by the University of Virginia, old C57BL/6J male mice (18 to 20 months old) had a poorer neurological outcome and more severe inflammation after transient focal brain ischemia than 8-week-old C57BL/6J male mice (young mice). They used LC Sciences’ 16S rRNA gene sequencing service on DNA extracted from fecal mice samples. Young mice with transplantation of old mouse gut microbiota had a worse neurological outcome, poorer survival curve, and more severe inflammation than young mice receiving young mouse gut microbiota transplantation. Old mice and young mice transplanted with old mouse gut microbiota had an increased level of blood valeric acid. Valeric acid worsened neurological outcome and heightened inflammatory response including blood interleukin-17 levels after brain ischemia. The increase of interleukin-17 caused by valeric acid was inhibited by a free fatty acid receptor 2 antagonist. Neutralizing interleukin-17 in the blood by its antibody improved neurological outcome and attenuated inflammatory response in mice with brain ischemia and receiving valeric acid. Old mice transplanted with young mouse feces had less body weight loss and better survival curve after brain ischemia than old mice transplanted with old mouse feces or old mice without fecal transplantation. These results suggest that the gut microbiota-valeric acid-interleukin-17 pathway contributes to the aging-related changes in the outcome after focal brain ischemia and response to stimulus. Valeric acid may activate free fatty acid receptor 2 to increase interleukin-17.
Aging-dependent gut microbiota changes and effects of fecal transplant on gut microbiota
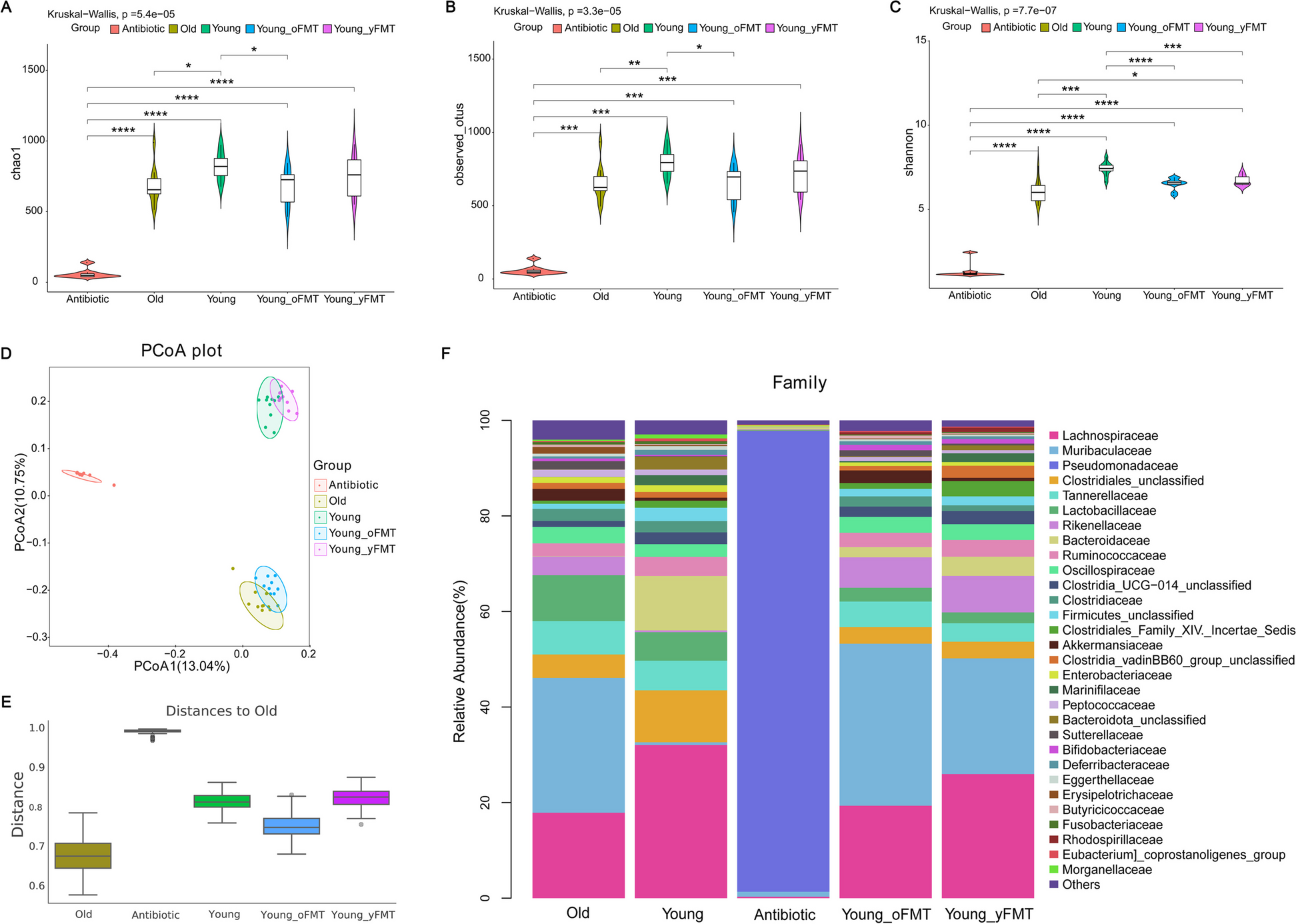
Feces were harvested from old mice (18 months old, n = 10), young mice (8 weeks old, n = 10), young mice 1 day after the completion of cefazolin treatment (n = 8) or young mice 14 days after receiving transplant of feces from young mice (Young-yFMT, n = 10) or from old mice (Young-oFMT, n = 10). The gut microbiota in these 5 groups of mice was analyzed and compared. A to C α diversity difference among the groups analyzed by chao1, observed_otus, and Shannon methods, respectively. D, E β diversity difference among the 5 groups analyzed by the PCoA and Anosim using Jaccard distance metrics, respectively. F stacked bar plot of relative abundance of taxa within gut microbiota at family level. * P < 0.05, ** P < 0.01, *** P < 0.001, and **** P < 0.0001
Zeng Xianzhang, Li Jun, Shan Weiran, Lai Zhongmeng, Zuo Zhiyi. (2023) Gut microbiota of old mice worsens neurological outcome after brain ischemia via increased valeric acid and IL-17 in the blood. Microbiome 11(1), 204. [article]
Aging is a significant risk factor for ischemic stroke and worsens its outcome. However, the mechanisms for this worsened neurological outcome with aging are not clearly defined. In a study led by the University of Virginia, old C57BL/6J male mice (18 to 20 months old) had a poorer neurological outcome and more severe inflammation after transient focal brain ischemia than 8-week-old C57BL/6J male mice (young mice). They used LC Sciences’ 16S rRNA gene sequencing service on DNA extracted from fecal mice samples. Young mice with transplantation of old mouse gut microbiota had a worse neurological outcome, poorer survival curve, and more severe inflammation than young mice receiving young mouse gut microbiota transplantation. Old mice and young mice transplanted with old mouse gut microbiota had an increased level of blood valeric acid. Valeric acid worsened neurological outcome and heightened inflammatory response including blood interleukin-17 levels after brain ischemia. The increase of interleukin-17 caused by valeric acid was inhibited by a free fatty acid receptor 2 antagonist. Neutralizing interleukin-17 in the blood by its antibody improved neurological outcome and attenuated inflammatory response in mice with brain ischemia and receiving valeric acid. Old mice transplanted with young mouse feces had less body weight loss and better survival curve after brain ischemia than old mice transplanted with old mouse feces or old mice without fecal transplantation. These results suggest that the gut microbiota-valeric acid-interleukin-17 pathway contributes to the aging-related changes in the outcome after focal brain ischemia and response to stimulus. Valeric acid may activate free fatty acid receptor 2 to increase interleukin-17.
Aging-dependent gut microbiota changes and effects of fecal transplant on gut microbiota
Feces were harvested from old mice (18 months old, n = 10), young mice (8 weeks old, n = 10), young mice 1 day after the completion of cefazolin treatment (n = 8) or young mice 14 days after receiving transplant of feces from young mice (Young-yFMT, n = 10) or from old mice (Young-oFMT, n = 10). The gut microbiota in these 5 groups of mice was analyzed and compared. A to C α diversity difference among the groups analyzed by chao1, observed_otus, and Shannon methods, respectively. D, E β diversity difference among the 5 groups analyzed by the PCoA and Anosim using Jaccard distance metrics, respectively. F stacked bar plot of relative abundance of taxa within gut microbiota at family level. * P < 0.05, ** P < 0.01, *** P < 0.001, and **** P < 0.0001
Zeng Xianzhang, Li Jun, Shan Weiran, Lai Zhongmeng, Zuo Zhiyi. (2023) Gut microbiota of old mice worsens neurological outcome after brain ischemia via increased valeric acid and IL-17 in the blood. Microbiome 11(1), 204. [article]